What is age-related macular degeneration?
Age-related macular degeneration (AMD) is a disease that affects a person’s central vision. AMD is the most common cause of severe vision loss among people age 50 and older. Only the center of vision is affected with this disease. It's rare that people go totally blind from it. But AMD can make it hard to read, drive, or do other daily activities that need detailed vision.
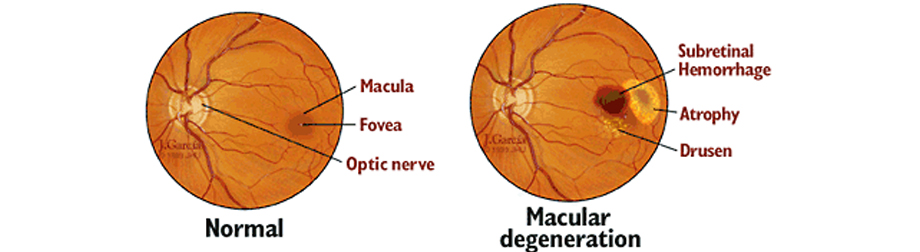
AMD occurs when the macula is damaged. The macula is located in the center of the retina and provides us with sight in the center of our field of vision. With less of the macula working, central vision begins to get worse.
What causes age-related macular degeneration?
What causes age-related macular degeneration?
- Dry AMD. This type is more common. The light-sensitive cells in the macula slowly break down. It generally happens in both eyes. It's thought that the age-related thickening of the tissue under the retina helps lead to dry AMD.
- Wet AMD. This type is less common. It accounts for most severe eyesight loss caused by AMD. New blood vessels behind the retina start to grow under the retina. They leak fluid and blood. They can create a large blind spot in the center of the visual field.
Who is at risk for macular degeneration?
Possible risk factors for AMD are:
- Being a woman
- Being age 60 and older
- Smoking
- Family history
- Uncontrolled high blood pressure (hypertension)
- Cardiovascular disease
- Obesity
- High blood cholesterol levels
- Farsightedness
- High C-reactive protein levels in the blood
What are the symptoms of age-related macular degeneration?
What are the symptoms of age-related macular degeneration?
- Blurry or fuzzy vision
- Straight lines look wavy
- Objects look smaller than they really are
- Colors look paler than normal
- A dark, empty area or blind spot in the central vision
- Quick loss of central vision, which is needed for driving, reading, recognizing faces, and doing close-up work
One of the most common early signs of AMD is tiny yellow deposits (drusen) in the retina. It may mean the eye is at risk for more severe AMD. Drusen will be visible to your eye care provider during an eye exam.
The symptoms of AMD may seem like other eye conditions. Talk with an eye care provider for a diagnosis.
How is age-related macular degeneration diagnosed?
In addition to a full health history and eye exam, your eye care provider may do these tests to diagnose AMD:
- Visual acuity test. The common eye chart test. It measures how clear and sharp your vision is.
- Pupil dilation. The pupil is widened with eye drops for a close-up exam of the retina.
- Amsler grid. This is used to find wet AMD. You are asked to look at a grid and see if straight lines in a grid pattern are missing or look wavy. Both of these may mean you have AMD.
- Fluorescein angiography. This test is used to find wet AMD. A special dye is injected into a vein in the arm. Pictures are then taken as the dye passes through the blood vessels in the retina. This helps the eye care provider evaluate if the blood vessels are leaking. It also helps the provider figure out if the leaking can be treated.
- Age-related macular degeneration (AMD) is a disease that affects the central vision.
- AMD can lead to severe loss of central vision. It rarely causes blindness.
- It can make it hard to read, drive, or do other things that need detailed vision.
- Risk factors include being age 50 and older, being a woman, smoking, high blood pressure, cardiovascular disease, obesity, and high cholesterol.
- There is no cure. But there are treatment choices that may stop or slow the disease progression.
- Know the reason for your visit and what you want to happen.
- Before your visit, write down questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your healthcare provider if you have questions.
How is age-related macular degeneration treated?
Treatment will depend on your symptoms, age, and general health. It will also depend on how severe the condition is.
Treatment for wet AMD often includes shots (injections) of medicine into the eye. This is done to stop the growth of the abnormal blood vessels under the macula. These injections are typically painless. Treatment may also include laser surgery. A high-energy beam of light is aimed directly onto the leaking blood vessels. This is done to stop further leaking. But this is often not needed.
Currently there is no treatment for dry AMD. But this does not mean that your sight will definitely be lost. Over time, central vision may be lost or reduced. Generally, the rate of loss is slow. There are nutritional treatment choices that may slow the disease progression.
What are possible complications of age-related macular degeneration?
AMD can result in severe loss of central vision. It rarely causes total blindness. But it can make it hard to read, drive, or do other daily activities that need detailed vision.
Living with macular degeneration
If you have already had some vision loss, talk with your provider. Ask for information on services for people with low vision. Also ask about devices that may help you with your daily tasks.
When should I call my eye care provider?
If your symptoms get worse or you have new symptoms, call your eye care provider.
Key points about age-related macular degeneration
Next steps
Tips to help you get the most from a visit to your healthcare provider:


